The Oral-Systemic Connection
In recent years, biomedical researchers have been exploring the major role inflammation plays in overall health, particularly in diseases of aging.
Immunology research is an area of expertise at ADA Forsyth. We examine the ways in which inflammation in the mouth, particularly periodontitis (or gum disease), is associated with a variety of systemic diseases, including diabetes, Sjogren’s syndrome, and Alzheimer’s.
Inflammation and Periodontitis
If left untreated, gum disease can cause extensive tooth loss, jawbone deterioration, and increased risk of developing systemic diseases. Mounting evidence suggests that inflammation plays a crucial role in periodontitis pathogenesis resulting in unregulated bone loss. Current treatments do not offer complete amelioration of periodontal tissue destruction because they do not directly address the biological causes of periodontal pathogenesis—unbalanced, overly aggressive immune responses.
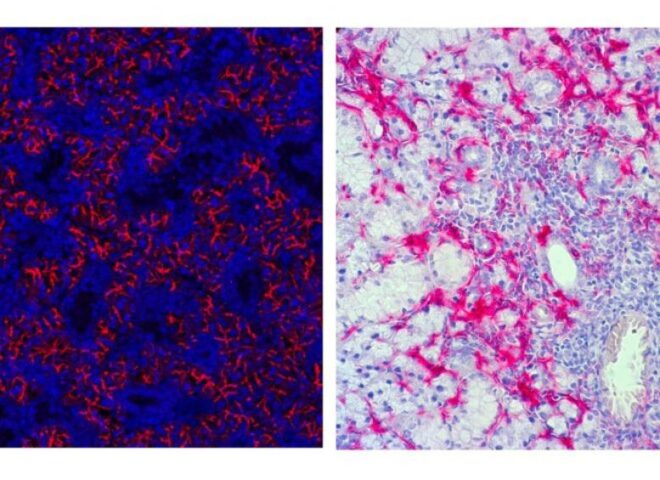
ADA Forsyth researchers are internationally known for their work on a new class of anti-inflammatory mediators produced by our own bodies, termed lipoxins and resolvins. These molecules actively resolve inflammation, which plays a major part in oral and systemic diseases, including gum disease, diabetes, and heart disease. Treatment of gum disease in animals with lipoxins and resolvins results in nearly complete regeneration, which has never been possible before. Stem cells are known to be very important in regeneration and new research at Forsyth is exploring how regulators of inflammation, such as lipoxins and resolvins, impact stem cells for potential new treatments.
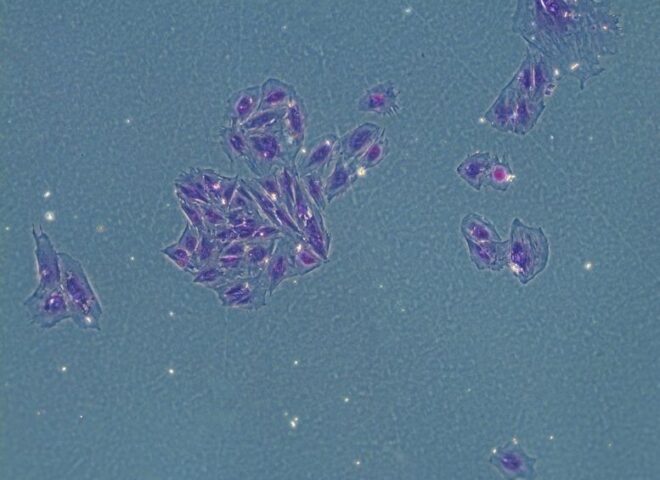
Scientists at ADA Forsyth are using animal models and in vitro methods to understand which molecule signaling pathways are major regulators of inflammation in periodontitis and how these pathways crosstalk. Other research focuses on host immune response in periodontal disease tissue destruction, particularly in the area of osteoimmunology—the interaction between the immune system and bone metabolism and its role in inflammatory bone destruction. The long-term goal of this work is to identify new therapeutic targets and develop novel, noninvasive, and sustainable immunological interventions to treat periodontitis.
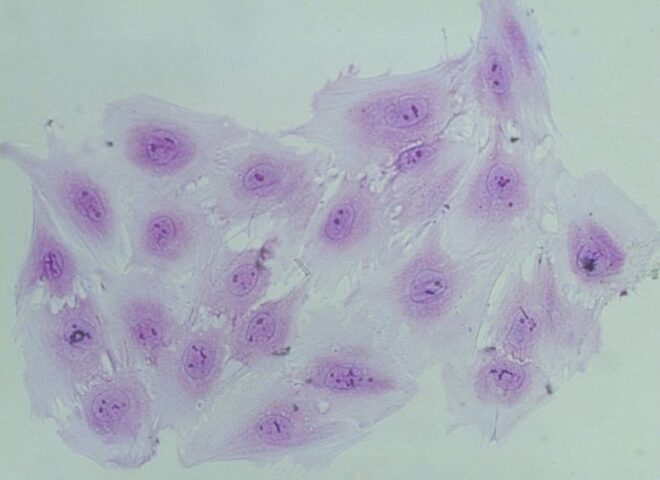
ADA Forsyth scientists are also working to develop targeted immunological interventions to treat periodontitis before it progresses to an expensive and unmanageable disease. This research is focused on B cells with a regulatory function, known as BREG, which play a key role in immune system balance by restraining excessive inflammatory responses.
Improving Root Canals
Root canals, which treat endodontic infections, are one of the most common dental procedures. Despite being performed regularly, nearly 15 percent of root canals fail, and patients require retreatment or tooth replacement. Researchers at ADA Forsyth are working to understand why these infections are so difficult to treat, with the ultimate goal of developing more effective treatment options.
ADA Forsyth scientists study the role of a protein called osteopontin (OPN), which has multiple effects on the body’s response to injury and inflammation. Researchers hope to use OPN to develop a new therapy to treat endodontic and other bacterial infections. This type of treatment would harness the body’s own response to infection and would be less invasive, costly, and unreliable than traditional dental surgeries.
Researchers at ADA Forsyth have also found that a type of molecule the body produces naturally, called a resolvin, can help regenerate pulp. Using resolvin to achieve pulp regeneration could potentially eliminate the need for root canals altogether.

Inflammation and Type 2 Diabetes
Researchers at ADA Forsyth are exploring the ways in which white blood cells regulate inflammation in patients with type 2 diabetes (T2D). While inflammation can play a protective role against injury and infection, it can also lead to health problems such as obesity, cardiovascular diseases, arthritis, blindness, chronic kidney disease, and periodontal disease.
Controlling chronic inflammation in the body leads to healthier outcomes for people with T2D. ADA Forsyth scientists are exploring the underlying causes of dysregulated inflammation and how it can be controlled, including how hyperglycemia and other metabolic changes can influence this phenomenon. Further understanding of inflammation regulation will be vitally important for innovations in personalized medicine and the development of novel treatment techniques—not just for T2D, but for the majority of chronic diseases, which are affected by inflammation.

Inflammation and Heart Disease
Scientists at ADA Forsyth have demonstrated that using an oral topical remedy to reduce inflammation associated with gum disease also results in the prevention of vascular inflammation and can lower the risk of heart attack. The active ingredient is an inflammation resolving molecule known as Resolvin E1. This research underscores the increasing body of evidence showing how inflammation in the mouth can have life-changing influences on other key systems in the body, such as the heart.
Sjӧgren’s Syndrome
Sjӧgren’s syndrome is a chronic autoimmune disease that affects 2-4 million Americans. Patients diagnosed with the syndrome experience dry mouth and dry eyes as a result of chronic inflammation and dysfunction of the salivary and lacrimal glands. One consequence of Sjӧgren’s syndrome is increased susceptibility to dental cavities. There is no cure for the disease and current treatment options primarily provide short-term relief from discomfort.
Researchers at ADA Forsyth are interested in understanding the immunological mechanisms underlying several systemic autoimmune diseases that affect oral health, including Sjӧgren’s syndrome. One major project investigates the protective and detrimental impact of different oral/gut microbial species and their metabolites on salivary gland function and Sjögren’s syndrome.
Another set of studies focus on simultaneously controlling autoimmune inflammation and enhancing salivary gland stem cell activity and salivary tissue regeneration. The ultimate goal of these lines of research is to develop effective and targeted therapeutic strategies for Sjögren’s disease and other autoimmune inflammatory conditions.