Fibromodulin, a matricellular proteoglycan, regulates myofibroblasts at the site of tissue closure to prevent excessive scarring
Somerville, Mass., 05/07/2025 – Cleft lip and/or cleft palate are among the most common craniofacial birth defects in the United States. These conditions, collectively referred to as orofacial clefts, occur when a baby’s lip or mouth do not form properly during pregnancy.
When an orofacial cleft is closed surgically, it commonly produces a raised, thick scar known as a hypertrophic scar, which can be disfiguring and affect function, with huge social and economic impacts to the patient.
A recent study from scientists at ADA Forsyth Institute (AFI) and University of California-Los Angeles (UCLA) suggests a new cutting-edge therapeutic approach may mitigate or even prevent excessive scarring, significantly advancing the field of wound healing and regeneration.
Scars are an important part of the body’s natural response to injury to wall off the injured site from normal tissues. During healing, scars are replaced gradually with healthy tissues. However, in abnormal healing, excessive myofibroblasts – cells that produce and organize collagen and play a key role in wound healing – and other abnormal activities can lead to excess scarring that does not heal normally.
A research team including AFI adjunct faculty Eric Kang Ting, D.M.D., D.Med.Sc., and UCLA researchers Chia Soo, M.D., Pin Ha, D.D.S., M.D., and Zhong Zheng, Ph.D. identified a molecule – fibromodulin (FMOD) protein – which works to maintain a balanced level of myofibroblasts, resulting in minimal scarring at the surgical site. The scientists detail this mechanism in a new paper published in Nature Communications.
“Our team has been exploring ways to improve scarring from cleft lip repair,” said Dr. Ting. “We have identified a new peptide drug derived from fibromodulin that may help reduce scarring. This publication demonstrates the broader role of fibromodulin in regulating a key cell involved in scarring: the myofibroblast.”

FMOD can prevent excessive scarring when included in surgical procedures that close tissue such as suturing of cleft lip. This method may also be successful in preventing keloid scars, a form of scarring that results in excess tissue growth beyond the boundaries of an original wound.
“By targeting the biology of scarring at the molecular level, this breakthrough has the potential to transform outcomes for patients undergoing cleft repair and other surgical procedures,” said AFI chief science officer and chief operating officer Ben Wu, D.D.S., Ph.D. “This powerful translational science brings fundamental biological insights to clinical care and would not have been possible without critical funding support by NIH.”
“Dr. Ting and I have been studying how to reduce skin scarring for the past two decades,” Dr. Soo said. “This recent breakthrough describing how fibromodulin may reduce excessive scarring through controlled cell death demonstrates a significant leap in potential treatments for patients with excessive scarring.”
The research offers a shift in perspective toward minimizing scarring and improving clinical outcomes in cutaneous wound repair. Dr. Zheng said, “in this study, we demonstrate that fibromodulin, a matricellular proteoglycan, accelerates the clearance of myofibroblasts without disrupting initial wound repair, providing a new mechanism to minimize scarring.” Dr. Zheng leads an FDA-approved clinical study currently in Phase 1/2A using a fibromodulin-derived peptide.
Additional collaborators on the project included Wenlu Jiang (UCLA), Xiaoxiao Pang (Chongqing Medical University), Chenshuang Li (University of Pennsylvania), Grace Xinlian Chang (UCLA), Yuxin Zhang (Chongqing Medical University), and Lawrence A. Bossong (Princeton University).
Funding:
This work was funded by NIH NIDCR R44DE024692 (to C.S. and Z.Z.) and SB1DE026972 (to K.T., C.S., and Z.Z.); NIH NIAMS R44AR064126 (to C.S. and Z.Z.), UCLA CTSI grant UL1TR000124 (to C.S.), UCLA Operation Mend (to C.S.), UCLA Orthopaedic Hospital (to C.S.), UCLA Orthopaedic Hospital Research Center (to C.S.), and the International Orthodontics Foundation.
Paper cited:
“Fibromodulin selectively accelerates myofibroblast apoptosis in cutaneous wounds by enhancing interleukin 1β signaling,” Nature Communications. DOI#1038/s41467-025-58906-z
###
About the ADA Forsyth Institute
The ADA Forsyth Institute was founded in 1910 as the Forsyth Dental Infirmary for Children (later, the Forsyth Institute), to provide dental care to the disadvantaged children of Boston. While continuing to serve children in need, yet recognizing the ultimate goal is to prevent dental disease, the Institute in 1915 began to focus on scientific research and is today the world’s leader in oral health research. In October of 2023, the Institute joined with the American Dental Association to form the ADA Forsyth Institute, a 501(c)(3) entity dedicated to improving people’s oral and overall health and powering the profession of dentistry through cutting-edge basic research, creative translational science, innovative clinical technologies, and global public health outreach. Consistent with the Institute’s founding mission, the ADA ForsythKids mobile dental program continues to serve children in need.
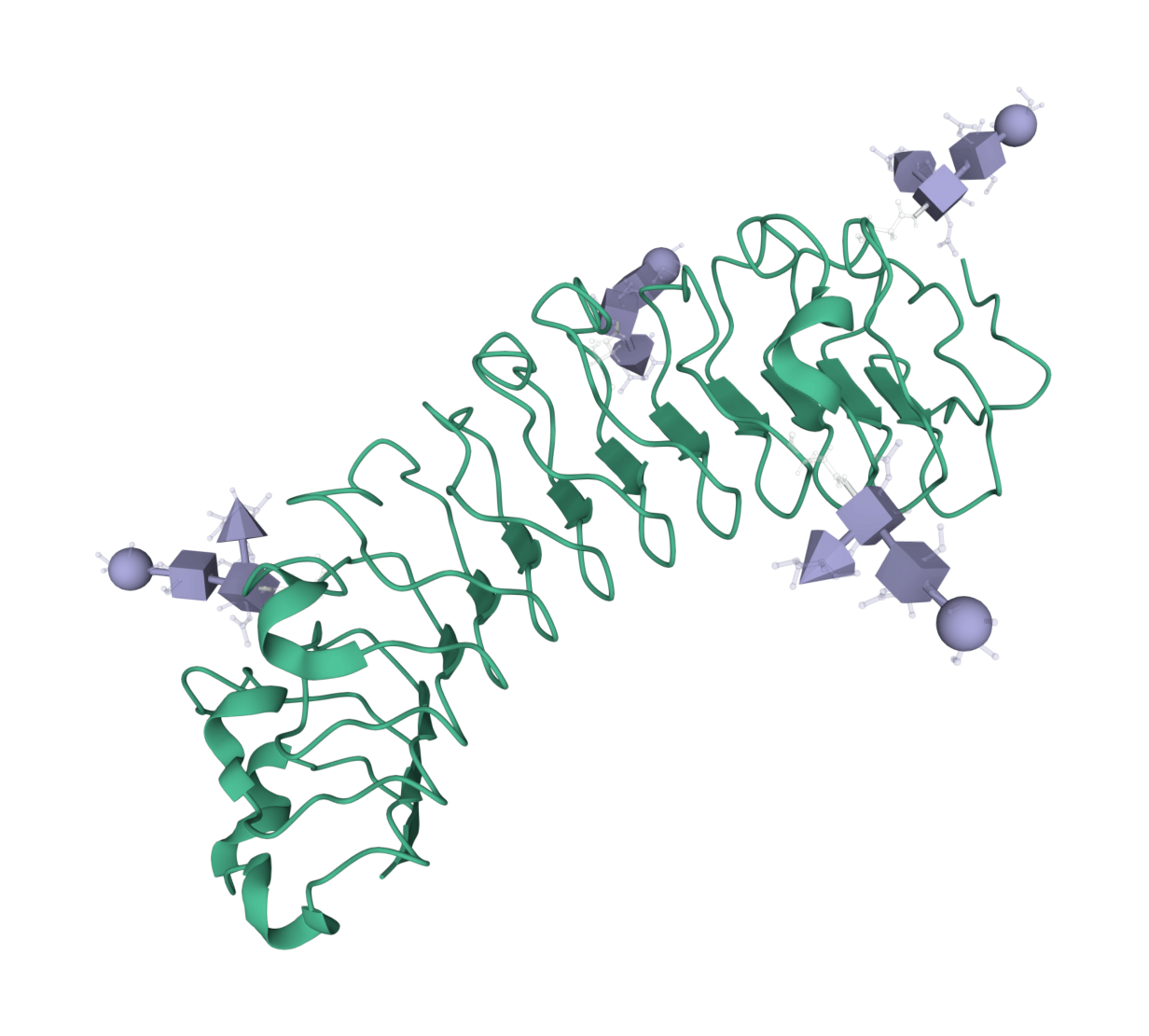
Image from the RCSB PDB (RCSB.org) of PDB ID 1BNA (H.R. Drew, R.M. Wing, T. Takano, C. Broka, S. Tanaka, K. Itakura, R.E.Dickerson, Structure of a B-DNA dodecamer: conformation and dynamics (1981) Proc.Natl.Acad.Sci.USA 78: 2179-2183).